About 70-75% of pregnant women decide to have an epidural during childbirth.1 The problem is that most of these women know little about epidurals, the procedure, and the benefits and risks when making this decision. Of course, I want every woman to have the desired birth they want. However, I want women to understand their available options to make better-informed decisions. Below, I’m sharing answers to frequently asked questions that I receive about epidurals. Hopefully, this information will help more women decide whether or not to get an epidural.
*Disclaimer: This post is not medical advice. As a birth professional, I get asked many of these questions regularly. So, I want to provide the answers I’ve found through my years of attending births, speaking to medical professionals and birth workers, and researching. I’m not saying that I’m for or against this procedure. I’ve recommended and encouraged epidurals at many births because they are medically necessary and/or best for the patient. I’m providing information about epidurals for women to feel more prepared before signing any release forms without reading the information.
What Is an Epidural?
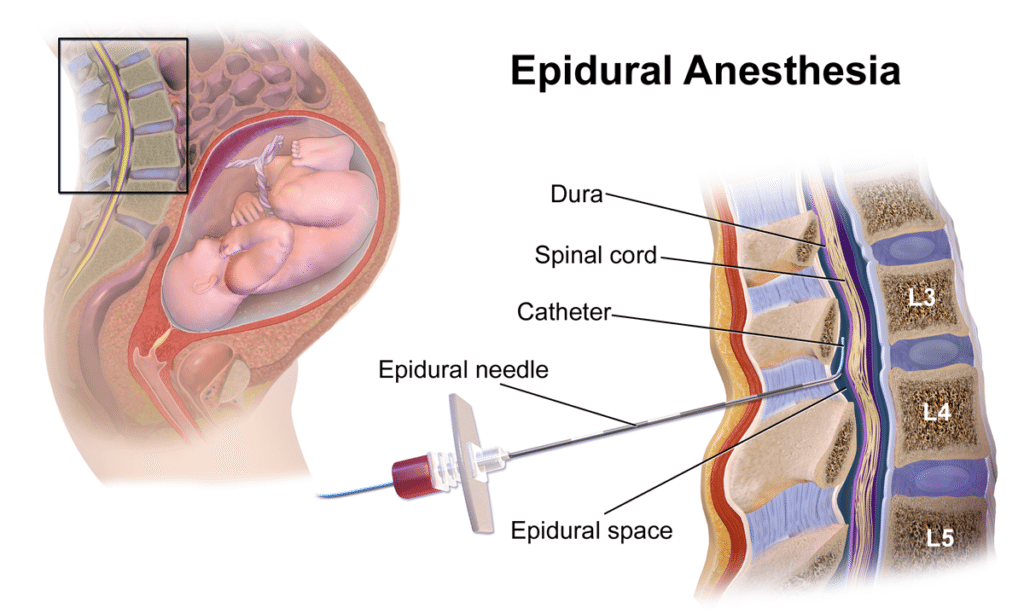
An epidural is when anesthetic medicine is injected into the lower part of your spine through a small, thin catheter inserted into your lower back. An anesthesiologist will place a small tube in the “epidural space” to help stop contraction pain during labor.16 Medication continuously flows through the small catheter.1 This blocks the pain of your contractions by numbing the nerves around your lower abdomen and pelvic floor.16
How Is an Epidural Performed?
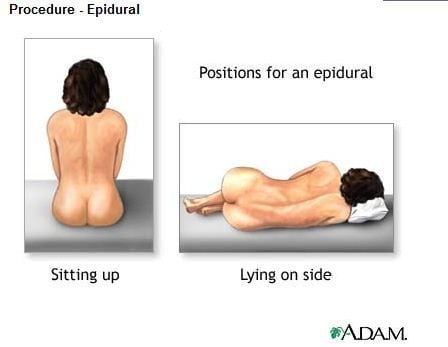
Once you’ve requested an epidural and the anesthesiologist has entered your room, all your guests will be asked to leave your labor and delivery room (except the hospital staff). In most hospitals, only medical staff can be in the room during the procedure. Your nurse will then help you lie on your side or sit up, and you will lean forward on a pillow to curve your spin to prepare for the procedure. (More than likely, you won’t be given a choice of which position you’d prefer.)
First, the anesthesiologist will clean your back with a cold liquid (iodine), then they will numb your lower back with a shot using lidocaine.2,3 The shot will feel like a bee sting.17 They do this first because they need your back to be numb before inserting the epidural catheter.16
Once your back is numb, the doctor will insert a hollow needle between the vertebrae in your lower back. You will feel pressure in your lower back when this is taking place.16,17 The doctor will then insert a thin tube through the middle of the needle and place it in your epidural space.4,16 They will then remove the needle, leaving the tube in place.16 You should feel no pain (only labor pain), or you might feel a funny sensation running down one of your legs for a second or two. It’s described as a “hitting your funny bone” feeling or like a rush or waterfall feeling down one leg.
A nurse will then tape the catheter up your back to stay in place. A pump connected to the catheter will continuously administer the anesthetic into the lower part of your abdomen to numb your lower body. You will be told to push the button attached to the pump every hour to control your dosage. This machine will only allow you to press it once every hour so that you don’t overmedicate yourself.1,16
What Drugs Are in an Epidural?
Each anesthesiologist has their own “recipe” for an epidural. They most commonly use a local anesthetic (like lidocaine or bupivacaine), maybe a pain reliever (like fentanyl), and something that boosts the effectiveness of those drugs (like epinephrine).5,6,7,8,22
What if I Move or Have a Contraction During an Epidural?
Contractions can be spaced out (three to five minutes or more) or be back-to-back.18 An epidural can still be placed regardless of how slow or fast your contractions are. If your contractions are more spread out, the anesthesiologist will wait until you’re finished with a contraction to do the procedure. But if you’re having contractions back-to-back, you can still get an epidural. Thankfully, the procedure isn’t so delicate that you must remain at a complete standstill. The doctor will still be able to place your epidural with slight movement. Your nurse will help you through each contraction as the epidural is placed to help you remain as still as possible.
How Long Until the Pain From the Contractions Stop?
Sometimes, it can take an hour (or longer) just for the anesthesiologist to arrive in your delivery room once you’ve requested an epidural. This is a worst-case scenario. Hopefully, they will arrive within 20 minutes. You may also need extra time to take IV fluid first, preventing your blood pressure from dropping too low before the anesthesiologist can start. An experienced anesthesiologist can take just five minutes to insert the epidural; a less experienced doctor could take up to 30-40 minutes. You should feel some of the effects within the first 10-15 minutes after the procedure.1 You will feel the full effect of the epidural after 20-30 minutes.16
Do Epidurals Always Work?
Not always.9 A good majority of them work for your entire labor. However, I’ve had several of my doula clients receive epidurals, and after a few hours of it working, it started wearing off. The anesthesiologist will come in to readjust or replace it, which should numb you and work again. I will warn you that I’ve seen epidurals fail even after the second placement. It might not work or could only numb one side of the body. Again, this is rare, but it does happen.9 I recommend you prepare by learning other pain relief techniques, just in case.
Will I Be Able To Walk Around After an Epidural?
No. Your lower body will be pretty numb, even if you feel like you can move your legs and feet.1 You won’t be able to carry yourself upright and walk with an epidural. Also, the hospital staff won’t allow you to leave the hospital bed once your epidural is in place. This is why you will have a bladder catheter in and the blood pressure cuff on. They will want to continuously monitor your contractions, your blood pressure, and the baby’s heartbeat every 15-30 minutes, so you must stay put.1,26
Can I Move Around at All With an Epidural?
You won’t be able to walk around. However, with the somewhat lighter/low-dose epidural, also known as a “walking epidural,” you should be able to move your position. But you still can’t walk around or leave the bed with this type of epidural.16 It will enable you to move your legs and toes, so you can sit up and move from laying on one side to another and not feel completely numb from the waist down.19
How Do I Go to the Bathroom?
An epidural causes numbness, so you won’t feel or know when your bladder is full. Instead, a nurse will insert a bladder catheter once your epidural is in place. This ensures that your bladder is being emptied.16,17
What Are the Positives of an Epidural?
There are several benefits of epidurals:
- It provides quick pain relief.16,22
- It’s a more effective pain reliever than analgesics (Stadol, Nubain, Demerol, etc.).10,11,12
- You will be able to rest — this is especially helpful if you have a long labor.21
- It can allow your body to relax and (potentially) open your cervix faster.20,22
- You will be more alert and be able to converse with your guests and hospital staff better.20,22
- It can help lower your blood pressure if it’s high.20
- If you need a C-section, you will be able to stay awake during the procedure and see your baby right away.16
What Are the Negatives of an Epidural?
Here are the potential risks of an epidural:
- Not all women feel total pain relief with epidurals.26 If you don’t feel pain relief within 30 minutes of having the procedure, ask your anesthetist to adjust the dose or try again.
- Sometimes, it can take a couple of tries to get the needle and tube in precisely the right place, which can be stressful.
- The hospital staff must monitor you continuously because your blood pressure can fall with an epidural. Someone will watch your baby’s heartbeat and take your blood pressure every 15-20 minutes.16,22,26
- Some women experience longer pushing stages when having an epidural since it reduces the urge to push. You may not feel an urge to push at all. This could mean you will have a higher risk of needing an assisted delivery with an episiotomy, forceps, or a ventouse, which is a vacuum device.16,22
- You may have side effects like shivering, headache, backache, dizziness, ringing in the ears, soreness, nausea, trouble urinating, or itchy skin.21,22,26
- In rare cases, a poorly inserted epidural could become infected.26
- Paralysis or long-term disability due to an epidural is extremely rare, and several safety measures will prevent that from happening. However, it’s still a risk, as with any medical procedure.16,23,24
- Epidurals can slow down labor if given in early labor, which may increase your chances of needing a C-section.
- Some women get a severe headache for several days afterward. This is caused by some spinal fluid leaking out when the needle is removed. It’s rare and occurs in only one in 100 cases, but it can happen.16,22
- The procedure can also increase your temperature and chances of developing a fever.1,16 This can confuse your doctor, who might not be able to tell whether the increase in temperature is because of the epidural (and not cause for concern) or an underlying infection that could transfer to your baby (chorioamnionitis).13
- Some women claim that they have had minor to severe backaches and back pain later on for weeks, months, or even years, though there isn’t clear evidence that an epidural causes chronic back pain.1,16,20,23,24
What Effect Will an Epidural Have On My Baby?
As for your baby’s health, the research is inconclusive regarding the effects of epidurals on babies. However, many studies show that after a mother has an epidural, their baby might have trouble latching on, leading to breastfeeding problems.14 Other studies show that a baby can experience symptoms like respiratory depression, fetal malpositioning, and increased fetal heart rate variability. This increases the need for forceps, vacuums, cesarean deliveries, and episiotomies.15,22 In addition, a mother having an epidural doesn’t seem to affect their baby’s Apgar scores.23
When Can I Have an Epidural?
You can have an epidural at any time during labor.1,16,20 However, most women choose to have one during active labor when they’re around 4-5 cm dilated or more.24 If you ask for one very late in labor — at 8 or 9 cm dilated (transition labor) — your doctor or midwife may advise against it because you’re so close to having your baby, and there’s a chance the epidural could slow the pushing stage.25
When Can’t I Have an Epidural?
Technically, you can always get an epidural. I’ve seen a woman get an epidural at 10 cm and ready to push. Of course, it’s not ideal at that time since you’re about to have your baby. But you can get one if you want one.
There are some conditions when an epidural wouldn’t be possible. You may be an unlikely candidate if:22,23
- You’re taking certain medications (such as blood thinners).
- Your blood work isn’t right (like having a low platelet count).
- Your anesthetist can’t find your epidural space (due to certain types of back surgery, scoliosis, weight, or back problems).
- You have an infection of the back.
With any medical intervention, there are risks. But, for many women, the benefits of epidurals outweigh the risks. This is your decision, and now you know what to expect. When you take your maternity hospital tour, I suggest seeing if you can meet with the anesthesiologist or at least get a copy of the hospital’s consent form. Knowing more information about epidurals can help you understand what you’re signing before dealing with contractions.
Epidurals are an excellent choice if you have a long, difficult birth and want pain relief. However, some people see the risks and prefer a natural birth (no pain medication). The great thing is — this is all your choice. Talk to your doula or healthcare provider for more information about epidurals. In addition, ask your doctor or midwife whether you’re a good candidate for the procedure.










