When thinking about your birth experience, you might consider getting an epidural while in labor. Epidurals are the most commonly used method of pain relief for labor in the United States.1 Many women plan on getting epidurals for pain management, but what are the benefits and risks? Should you wait or not wait to get one? Read on to learn more about when to get an epidural during labor.
What Is an Epidural?
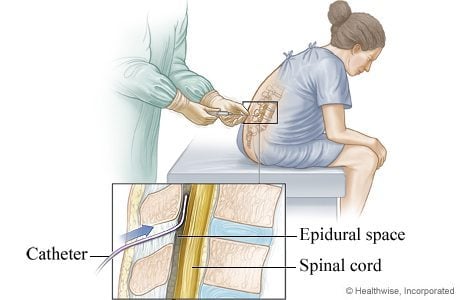
An epidural delivers pain relief medication continuously to your lower body and blocks labor pain. The medicine goes through a catheter, which is a skinny and flexible tube. An anesthesiologist inserts the catheter into the laboring mother’s epidural space in her lower back.1
Benefits of Epidurals
Here are some of the benefits of getting an epidural:1,5
- It allows you to rest if your labor is lasting too long.
- It helps reduce the discomforts of childbirth so women can have a more comfortable and positive birth experience.
- If you deliver by cesarean, an epidural will allow you to stay awake to see your baby.
- After a cesarean, an epidural will also provide effective pain relief during recovery.
- If you tear during pushing, your epidural numbs your perineum while your doctor is stitching.
- When other coping techniques are no longer helping, an epidural can help you deal with feeling exhausted and irritable.
- An epidural can allow you to relax and focus so that you can continue in your birth experience.
Risks of Epidurals
Like any intervention, epidurals also have risks. For instance, you might experience the following side effects with an epidural: shivering/shaking, ringing of the ears, itching, backache, soreness at the site of the needle insertion, nausea, and trouble urinating. In addition, your lower body may be numb for a few hours after birth, so you’ll need assistance to walk. In rare cases, you can have permanent nerve damage where the catheter was inserted.1,5
Here are some of the other risks of getting an epidural:
Drop in Blood Pressure
An epidural can cause your blood pressure to drop, which would require the use of IV fluids, medications, and oxygen. Your medical team will check your blood pressure routinely (about every 15-30 minutes). This helps them ensure the proper blood flow to your baby.1
Headache
Epidurals might cause a severe headache due to the leakage of spinal fluid. However, there’s a relatively small chance this can happen, as less than 1% of women experience this side effect. But if your symptoms do persist, your medical team may perform a blood patch (a procedure where blood is injected into the epidural space to stop the leaking) to relieve your headache.1,2
Frequently Changing Positions
After your epidural is placed, you won’t be able to get out of bed. This means you’ll need to alternate sides while lying down. You’ll also have continuous fetal monitoring so your medical team can check for changes in the fetal heart rate. You need to alternate sides as well. Rotating sides ensures your epidural medication is evenly dispersed throughout your lower body. Due to gravity, if you lie on one side for too long, the bottom side of your body will become numb and heavy while the top side will regain more feeling.1
Difficulty Pushing
An epidural can make it more difficult for you to push during labor. Because of this, you may need additional medications or interventions, such as a vacuum, an episiotomy, forceps, or a cesarean. When creating your birth plan, you and your doctor can discuss what interventions they may use in these cases. You can also request to turn off the epidural when pushing. This allows you to feel where and how to push more effectively, which can help you avoid other second-stage interventions.1,12
Issues With Baby
With an epidural, some babies will have trouble latching on, making it difficult for mothers to breastfeed.1,3 However, the overall evidence is conflicting, and it’s very difficult to compare the various studies evaluating the impact of epidurals and breastfeeding. Some show a positive impact, while others show no impact or even a negative impact.13
A baby might also experience respiratory depression, fetal malpositioning, and increased fetal heart rate variability. This increases the need for forceps, vacuums, cesarean deliveries, and episiotomies.1
When To Get an Epidural During Labor
Now you know some of the benefits and risks of having an epidural. If you’ve decided you want one, the question is: when is the right time to get one in labor? Is there even a right time to get it? One doctor may say getting an epidural is fine as soon as you get to the hospital. Another might say you need to be in active labor and at least 3, 4, or 5 centimeters dilated before they’ll call the anesthesiologist. So, what’s the right answer? Honestly, both answers may be the right choice for you.
The bottom line is that you shouldn’t be denied pain control at any point during your labor course when you desire it, and when you ask for an epidural, it should be provided. ACOG supports this and offers the following statement:14
“There is no other circumstance in which it is considered acceptable for an individual to experience untreated severe pain, amenable to safe intervention, while under a physician’s care. In the absence of a medical contraindication, maternal request is a sufficient medical indication for pain relief during labor. Pain management should be provided whenever medically indicated.”
After being at many hospital births and supporting women through all types of deliveries, I’ve noticed similar patterns and outcomes when women get epidurals too early. I’ve seen that waiting until your cervix has dilated to at least 4 centimeters before you call for an epidural is beneficial.1,7 At this point, your body has established active labor. This means strong and continuous contractions, so it’s more likely for things to continue to progress.8 As a result, you reduce your chances of needing more medical interventions and reduce your chances of a C-section.4
Myths, Facts, and Uncertainties
With approximately 60% of laboring women opting for epidural analgesia, there’s no doubt that questions arise about its impact on the birthing process.15 Let’s shed some light on what’s confirmed, debunked, and uncertain:
1. TRUE: Epidurals Are Associated With Prolonged Labor
In my experience, women who had received an epidural before they had a strong, consistent labor pattern and minimal cervical dilation experienced their labor slowing down. This resulted in them needing Pitocin to help increase and strengthen their contractions. When your labor slows down, this prolongs your labor and your baby’s birth. And unfortunately, this leaves more time for potential problems to arise.9,15,17
However, the facts are that the effects of epidural analgesia and its impact on labor progression have been extensively studied. There’s no impact on the length of the first stage, and the second stage of labor was only lengthened by approximately 15 minutes.15
2. MYTH: Epidurals May Increase Your Risk of a Cesarean Section
It isn’t true that epidurals increase your risk of cesarean section, and several studies support this. For instance, a Cochrane review analyzed 27 trials on the effects of epidural analgesia on cesarean rates and found no effect on the overall risk of cesarean delivery.16
3. TRUE: Epidurals May Increase Your Risk of an Operative Delivery
Getting an epidural during labor might increase the chances of needing instruments like forceps or vacuum assistance to deliver the baby. This could be because the epidural might affect how effectively the mom pushes or baby’s ability to move into the right position for birth.16
4. UNCERTAIN: Epidurals Cause Fetal Malposition
There’s uncertainty about whether getting an epidural during labor could cause baby to be in a less ideal position for birth. Some studies suggest that epidurals might be linked to the baby’s head not turning to the best position for delivery, but other studies haven’t reached a clear conclusion on this. Additionally, some experts think that starting epidural pain relief early in labor might increase the risk of baby being in an unfavorable position, compared to starting it later.15,16
At the end of the day, this is your body, your baby, and your birth experience. You have a better understanding of what’s right for you. And you get to choose when you want an epidural. Your care provider might give you their opinion, but it’s your choice. Now that you know all this information, you can make an informed decision.
I recommend listening to your body and making the best choice for you, whatever and whenever that is. This is why I say either option is right for when you decide to get an epidural — whether you get it at the beginning of labor or later. They’re both good options because you’ve made the best decision for yourself. 🙂






























