The term “nipple confusion” makes many breastfeeding moms cringe. Nipple confusion describes a baby’s struggle in changing back and forth from different feeding mechanisms, breast to bottle, and vice versa. There is much debate that surrounds nipple confusion. Is the baby really “confused” by the mother’s nipple and a bottle nipple? How does this happen?
The idea of nipple confusion may be worrisome to many breastfeeding mothers. Bottles and other feeding methods may be medically necessary for certain instances or need to be introduced for different reasons. If nipple confusion is a concern or you are currently going through this phase with your little one, keep reading. Below is an explanation and some tips that may help you navigate this struggle.
What is Nipple Confusion and Why Does It Happen?
Nipple confusion is a term used to explain a baby’s difficulty switching feeding modes, most commonly from the bottle back to the breast. A baby may start to prefer a specific feeding method. If you find your baby is starting to refuse to breastfeed after being introduced to the bottle, you may start feeling overwhelmed and stressed.
The nipple of a breast is very different from the nipple of a bottle. Texture, size, rigidity, it all differs. If a mother has inverted or flat nipples,8,11 or even non-elastic nipples, the baby may find immediate relief when given a bottle for the first time. The baby may refuse the mom’s breasts when offered again because the bottle provided a more satisfying feeding experience than what the baby was used to.1
Another difference between a mother’s nipple and a bottle nipple is the flow each offers. When babies are breastfeeding, they latch, begin suckling, and wait for the mother’s let-down. A let-down is when the milk starts to push out of the mother’s breast once the baby has been suckling.2 In contrast, when a baby feeds from a bottle, the milk flows freely immediately. One study noted that this “instant gratification” from bottle feeding could be an influencing factor in nipple confusion.3 As you can see, there are many factors that play a role in leading to what many call nipple confusion.
Is Nipple Confusion Real?
Some believe nipple confusion might be the wrong term to describe what is happening.3 Many breastfed babies have a reason why they are offered a bottle. The baby’s oral anatomy or the mother’s breast anatomy are common barriers to the bottle’s introduction.1 An example of an oral anomaly that may cause breastfeeding difficulty is ankyloglossia, also known as a tongue tie.4
Regardless of anatomy, a factor that makes breastfeeding hard for the baby may be how easy it is to feed from a bottle. When breastfeeding is challenging, and the baby is presented with a bottle, they may feel the bottle is more satisfying to feed from than the breast. This can create problems returning to the breast, especially if the original influencing factor is not corrected. Therefore, some practitioners believe it is not nipple confusion but rather a preference.1
Every mother and baby breastfeeding duo is unique. Some babies may easily go back and forth between bottle and breast, never missing a beat. Others may need additional support. You should contact a lactation consultant for guidance if you are having trouble.
Signs of Nipple Confusion
Babies can be obvious when showing a feeding preference. If your baby is bottle feeding and has difficulty returning to the breast, you may recognize that they are very reluctant to breastfeed. Latching may be difficult, and they may start to cry each time you offer your breast. If your baby can latch, you might observe an uncoordinated sucking pattern, causing ineffective milk removal.5 These are just a few signs your baby may be experiencing nipple preference after you introduce them to a bottle.
There is no way to predict if your baby may have a nipple preference when changing feeding modes, but some say a preterm infant may be more susceptible. A preterm infant may have a weaker suck, making the bottle’s flow more accessible and more satisfying for the baby.6
How Can I Avoid Nipple Confusion?
If you wish to introduce a bottle to your baby for medical or personal reasons, there are a few tips to consider in assisting in preventing nipple confusion for your baby.
Establish Your Breastfeeding Relationship
Make sure both you and baby are feeling comfortable with breastfeeding and baby can successfully latch and remove milk without any struggles. It is recommended not to introduce the bottle until around four weeks after birth.7
Consider Alternative Feeding Methods
An alternative feeding method might be best for you and your baby. Discuss possible options with your health care team to assess which way might be best. Some alternative feeding methods include:
Finger Feeding
A suitable short-term method to help a baby receive expressed milk. The caregiver uses a syringe and sometimes a feeding tube set up along the finger to feed the baby. Finger feeding allows the baby to use the sucking reflex.1
Cup Feeding
Using a small cup with a smooth rim, slowly tilt the cup until milk begins to hit the baby’s lip. Baby will start to use their tongue to sip the milk. This avoids exposing the baby to an artificial nipple.1
Paced Bottle Feeding
Keep the bottle horizontal when feeding the baby, enforcing that the baby still needs to suck to retrieve milk and slowing the flow. Paced bottle-feeding is a good practice if you need to use a bottle.1
Supplemental Nursing System
A device that uses a tube to deliver milk while secured by the mother’s nipple.7
Tips to Prevent Nipple Confusion
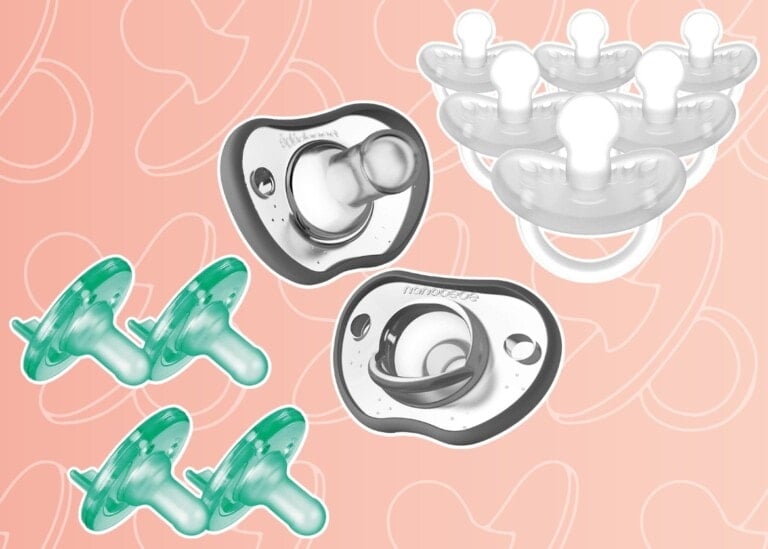
Avoid or postpone introducing a pacifier: Babies love to suck to both feed and soothe. A pacifier is another form of a “nipple” commonly used to soothe a baby, but while doing this, it can stretch out the time between the baby’s feeds, causing the baby to feed less frequently. This artificial nipple, like a bottle, varies in texture, shape, and size. The American Academy of Pediatrics recommends caregivers introduce a pacifier after establishing breastfeeding, usually around 3-4 weeks.10
Work with a lactation consultant: Get evaluated early by a lactation consultant. Most hospitals will have a lactation team available to offer support before your discharge home. They can ensure the baby is latching well and breastfeeding effectively. Learning what positions work best for you and your baby can help you feel more confident in feeding your baby. A solid start to breastfeeding can lead to success down the road.
Overcoming Confusion
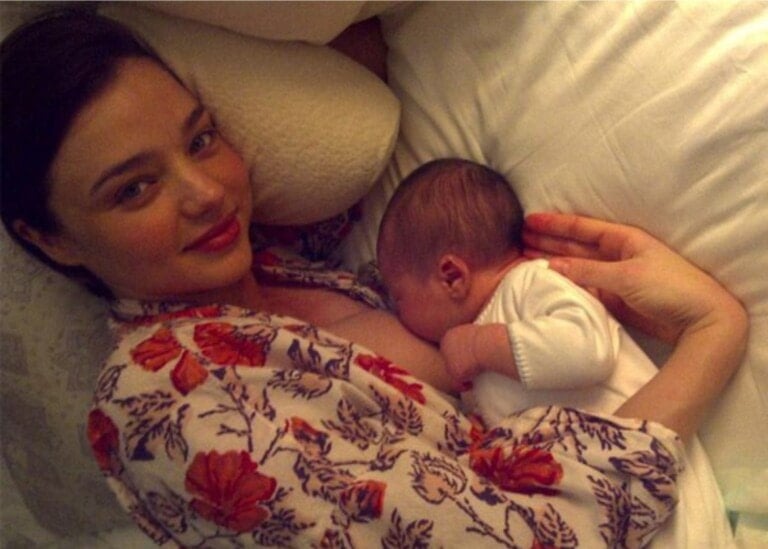
Although a baby refuses to breastfeed after being bottle-fed, there are ways to support your baby when returning to the breast. It may just take some time and support. This may feel overwhelming, but the most important tip is to stay calm for yourself and your baby. Next, practice skin-to-skin. Skin-to-skin bonding is a very simple yet powerful way to support your breastfeeding journey.5
Continuing to offer your breast to your baby is very important.5 When attempting to breastfeed, ensure your baby is showing hunger cues and that they are ready to eat. Identify early cues like them putting their hands to their mouth or if they turn their head toward the breast. Do not wait until the baby is crying. This is a late cue and could cause challenges with latching. Before attempting to latch, hand express9 (a technique used to push the milk out of the breast using your hand) some milk so the baby gets an instant taste of breastmilk, encouraging them to latch and begin suckling.
Once the baby latches, they may recognize that the flow is slower than with a bottle. Breast compressions are a great idea to help keep milk flowing, which may be what your baby becomes accustomed to with the bottle. To do breast compressions, you use your hand to hold your breast in a cupped position, or C shape. Squeeze and compress your breast to help the flow of milk. When milk is constant, your baby will be swallowing, which encourages suckling. This can help keep your baby satisfied at the breast and keep them sucking.5
Lactation Consultants Can Help
Meeting with a lactation consultant could be beneficial if you are not finding success in navigating this struggle on your own. Lactation consultants are well versed in all things breastfeeding. They will be able to assess mom and baby breastfeeding. They can offer feedback, help with positioning and the baby’s latch, and can help identify any underlying factors that may be the root cause of the baby’s nipple confusion.
Suppose a consultant identifies a problem that may cause the baby’s preference for a bottle. In that case, the lactation consultant may be able to assist in correcting or offering a solution. For example, if the mother has flat nipples, the baby is most likely having trouble latching and feeling satisfied with breastfeeding. A nipple shield can be an excellent tool for a mom with flat nipples. The shield gives the baby more of an area to latch onto. Nipple shields can be difficult to use; the lactation consultant will be able to educate and give hands-on support to help you learn how to use this device to get your baby back to the breast.10
In overcoming your baby’s struggle with breastfeeding, it is essential to pump your breasts. Breastfeeding is already challenging; you do not want to add a low milk supply to your list of concerns. Your breasts must have milk removed to maintain your supply and to meet your little one’s needs.
Nipple confusion can be stressful for the mother and baby. It is important to know that although your baby may be struggling now, this can be temporary. Many bottle-fed babies learn to breastfeed again once problems are resolved.1 So be kind to yourself, stay relaxed, and please don’t be afraid to reach out to your healthcare team for more support!