Breastfeeding discomforts can be quite a literal pain when they pop up. Caring for your baby while dealing with breastfeeding discomforts and concerns can be overwhelming and tiring. Some common breastfeeding difficulties may or may not present themselves during your journey. By being aware of these discomforts and knowing how to manage them, you will be prepared and set yourself up for success.
7 Common Breastfeeding Discomforts
Let’s dive into seven common causes of breastfeeding discomforts and recommendations for handling them if they arise.
1. Clogged Ducts & Engorgement
While engorgement and clogged ducts are technically two different discomforts, they are related.
Engorgement
Engorgement of the breasts can refer to both edema of the breasts and milk stasis. Edema can commonly occur when a mother has a quick and sudden increase in her milk supply or has increased volumes of intravenous (IV) fluids during labor.1,2 Both can cause increased fluid to build in the breasts, resulting in engorgement. This increased fluid can impact milk ducts, not allowing them to fully dilate and leading to milk stasis.1
Another form of engorgement is a result of milk stasis. Milk stasis occurs when the mother’s breasts are full of breast milk and have not been emptied as needed. Milk stasis can lead to further problems, such as plugged milk ducts and mastitis, and impact milk supply if not addressed and taken care of.1
Because of edema and milk stasis, engorgement can cause a mother’s breasts to feel tender and sometimes painful, firm, warm, and red.2 It can make breastfeeding extra challenging, especially regarding baby latching.
How To Manage Engorgement
Recommendations to manage engorgement include the following:
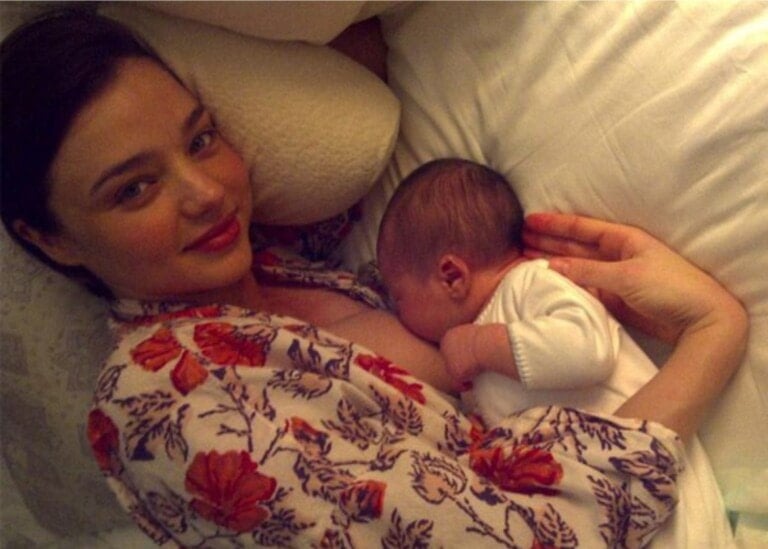
- Skin-to-skin contact with mother and baby to encourage breastfeeding.1
- Ensure the baby is latching correctly to adequately remove milk from the mother’s breasts.1
- Frequent removal of milk from the breast. This can be done by baby breastfeeding or expressing milk.2
- Reversed pressure softening technique. This allows the mother to help with edema around the areola, making latching for the baby easier and allowing them to remove milk adequately.1,2
- Cold pack application for 20-minute intervals.2
- Anti-inflammatory medications. Make sure to speak with your healthcare provider before taking it.2
- Lymphatic drainage. This is a technique to help move fluid and decrease edema.2
- Consultation with a lactation specialist for management guidance.
Clogged Ducts
Clogged ducts, also known as plugged milk ducts or ductal narrowing, occur when factors such as breast engorgement cause milk ducts to be compressed and narrow. Plugged milk ducts can present as tender lumps in the breast and can cause warmth, redness, and increased discomfort.1 If ductal narrowing is left untreated, it can lead to mastitis.2
How To Manage Clogged Ducts
Recommendations to manage clogged ducts include the following:
- Breastfeed baby on demand.1,2
- Wear loose-fitting clothing, and do not wear restricting bras or bras with underwire.1,2
- Sunflower lecithin daily can help. Reach out to your healthcare team for help with correct dosing.2
- Avoid over-pumping, as this can worsen things and cause an oversupply of breast milk.2
- Avoid deep massage; this can cause harm and injure the breast.2
2. Mastitis
Just hearing the term mastitis can make you cringe. It is a breastfeeding discomfort that everyone hopes they can avoid. Mastitis can develop when ductal narrowing occurs in the breast due to inflammation, edema, and other contributing factors.2 Mastitis can present as flu-like symptoms such as fever, increased heart rate, and chills and can cause a painful area in the breast that is red and swollen.2 Some forms of mastitis may require treatment with antibiotics.
How To Manage Mastitis
Some recommendations to manage mastitis include the following:
- Continue to breastfeed your baby. It is recommended to continue to bring your baby to your breast for feedings even while managing and treating mastitis.2
- Consult with your healthcare team. They will be able to evaluate your symptoms, and they may prescribe antibiotics for bacterial mastitis.2
3. Nipple Pain
Are you experiencing nipple pain? Stop what you are doing, and let’s dive into how your baby is latching. Many newly breastfeeding mothers do not realize the importance of “properly” latching your little one to the breast. If your baby does not have a deep latch, it is common for moms to experience nipple pain and discomfort. First-time breastfeeding moms may not know what a “good latch” should look or feel like. This is why many moms may experience nipple pain at the start of their breastfeeding journey. Learning a “good latch” can take time and practice for you and your baby, but with support and education, you can navigate this discomfort and breastfeed without nipple pain.
How To Manage Nipple Pain
Here are several recommendations for managing nipple pain:
- Work on a “good latch.” Some signs of a proper breastfeeding latch may include pain-free breastfeeding with the mother and baby being comfortable, the baby latching on with a wide mouth, and covering most of the areola, not only the nipple, the baby’s lips are flanged out on the breast, and you can visibly see or hear baby swallowing breastmilk.3
- When experiencing nipple pain, consulting with a lactation specialist is always helpful. The consultant can evaluate how your baby latches to your breast and show you the correct way to latch. Pain can start due to a shallow latch, with the baby just sucking on the nipple. They may also evaluate your little one’s suck and oral anatomy to identify contributing factors that may impact latching.1
- Find the breastfeeding position that works best for you and your baby. There are many “holds” you can try. It is also helpful to use a breastfeeding pillow to support your baby and also help you feel more comfortable and not “slouched” over.1
- If your nipples have visible cracks and trauma, take measures to treat them.1
4. Let Down Discomfort and Pain
Some women will experience discomfort or pain when they “let down.” For many who experience this, it lasts about the first month of breastfeeding.1 A mother with a strong milk ejection reflex might experience sharp pain in the breast as her milk begins flowing.1 For others, this discomfort can result from numerous reasons, such as having an oversupply of breast milk, engorgement, an infection, plugged ducts, or even an injury.4
How To Manage Let Down Discomfort and Pain
Here are several recommendations to help you manage discomfort and pain with let down:
- Find a comfortable, supportive, and relaxed position to breastfeed.4
- Address concerns that may be causing letdown pain.4
- Hand express a small amount of breastmilk, then latch baby.1
- Consult with a lactation specialist for guidance and support.
5. Thrush or Yeast Infection
When thrush is untreated, it can spread quickly. This could even mean the yeast can spread to your nipples if your baby has untreated oral thrush.5 If you are experiencing a yeast infection on your nipples, the skin on your areola and nipple may look irritated and inflamed and cause you pain while feeding and in between feedings.1
How To Manage Thrush
Recommendations to manage thrush or a yeast infection include the following:
- Reach out to a healthcare provider for an evaluation and treatment plan.1
- Rinse the nipple area with water before and after feeding your little one.1
- If breastfeeding is painful, express breast milk for your baby until the pain resolves; otherwise, you may continue breastfeeding.1,5
- If thrush is suspected in the baby, consult your pediatrician for a treatment plan.6
6. Biting Baby
There comes an age when your baby may start to bite while breastfeeding, and this is not only a painful discomfort but can be pretty shocking. As your baby gets older, distractions become commonplace when breastfeeding. Any little noise or movement may catch their eye, and they do not want to miss out on the fun. This may cause them to clamp down and pull your nipple as they quickly turn one way or another.5
How To Manage a Biting Baby
Here are some recommendations on how to handle it when your baby bites:
Firmly state “Don’t bite” or “no bite.” Never yell; it may surprise you, but your baby never tries to hurt you.5,7
Remove your baby from your breast and again state, “no bite.” Return baby to the breast if still feeding; if finished, you may offer a teether to chew on.7
If the nipple experiences trauma and the skin is broken, use basic first aid and treat the wound.5
Watch your baby’s cues, and anticipate if your baby is becoming distracted; remove from the breast if finished feeding.7
7. Feeding After C-Section
Having a Cesarean section is a major surgery.1 As with any major surgery, you may initially experience pain and continued discomfort at your incision site for some time. Healing from surgery, alongside taking care of your infant and breastfeeding, can feel overwhelming. This is a great time to accept help from your support system.
How To Manage Feeding After Having a C-Section
Here are some recommendations for how to manage breastfeeding your baby after a C-section:
- Ask for help. When first breastfeeding after delivery, you may need extra support from your significant other and your healthcare team. In addition, ask for guidance and assistance with comfort when breastfeeding.
- Find a comfortable breastfeeding position for you and your baby to breastfeed; the football hold position is an excellent place to start.9
- Use lots of pillows for support and to protect your incision while feeding.8
- Skin-to-skin is always a good idea!
- Pain medication. Speak with your healthcare team for appropriate pain medication to help you feel comfortable after a C-section.8
These breastfeeding discomforts are never anything a new mom wishes for herself. Although they may be stressful, you should never suffer alone. So, contact your healthcare team and lactation specialist for assistance in problem-solving your discomforts so you are no longer in pain and are breastfeeding in comfort!