Mastitis is a term that terrifies many breastfeeding moms. Maybe you have experienced it, had a friend who has, or you worry you might develop it. The symptoms of mastitis can be very uncomfortable and increase stress levels during your breastfeeding journey. And the last thing a breastfeeding mom needs is additional stress. Knowledge of mastitis can help you identify early signs, know potential risk factors, and empower you to reach out to your lactation team or healthcare provider if you need help. Although mastitis is quite literally a “pain,” it does not have to be the end of your breastfeeding journey.
What Is Mastitis?
Mastitis is a breastfeeding complication that occurs when a mom experiences inflammation in her breast. It is commonly accompanied by a high fever and flu-like symptoms and can cause breast pain and tenderness, often in one breast in a localized area. For most women who develop mastitis, it occurs in the first six weeks postpartum, but it can develop anytime.1,2
Mastitis presents on the spectrum from mild to severe. When identified and treated early, your healthcare provider can stop the progression of severity. The American Academy of Breastfeeding Medicine (ABM) revised its protocol on mastitis in 2022 and identified a spectrum of inflammatory conditions within the lactating breast that can occur. This includes detailed information on ways to treat and manage a mastitis diagnosis.4
Risk Factors Associated with Mastitis
Although we can never predict who will develop mastitis, some factors may put you at a higher risk.2
- Oversupply of milk
- Rapid weaning
- Previous cases of mastitis
- Stress and fatigue
- Frequently plugged ducts
- Breast engorgement
- Trauma to the breast
- Wearing tight bras
- Nipple damage
What Causes Mastitis?
When inflammation starts in the breast, problems can arise. The Mastitis Spectrum protocol by the ABM identifies the progression of inflammatory processes in the lactating breast that can cause mild to more severe cases of mastitis.4
Hyperlactation and Ductal Narrowing
Hyperlactation, also known as an oversupply of breast milk, is a common cause of breast inflammation. When a woman produces an oversupply of breast milk, it can cause edema and puts her at a higher risk of disrupting the breast microbiome. When these factors are at play, the mastitis spectrum continues, and you will next see the breast’s ductal lumens become more narrow.4
So, what is ductal narrowing? This is more commonly called a plugged duct or inflammation of your ducts. There are many ducts in a breast, and when narrowing occurs, you may feel breast tenderness and some redness. If the narrowing worsens, the mastitis spectrum progresses and can lead to inflammatory mastitis.4
Inflammatory Mastitis
With inflammatory mastitis, the inflammation has progressed in your breast, which is now swollen, red, and painful. You’ll feel terrible and have flu-like symptoms. This form of mastitis can occur without an infection being present.4
Bacterial Mastitis
As inflammation progresses in the breast and symptoms continue, bacterial mastitis becomes the likely culprit of your pain. Unfortunately, at this stage, it is common for your symptoms to progress further. You may even notice the redness and edema spreading further around your breast.4
Let’s start with some good news. Bacterial mastitis is not contagious, and research has shown that you can continue to breastfeed your full-term, healthy baby. The not-so-great news is you now get to start a round of antibiotics. Common pathogens in bacterial mastitis are forms of staphylococcus and streptococcus.4
Abscess
An abscess can form if you don’t control and treat bacterial mastitis. An abscess is an infected area of fluid and can usually be felt when touching the breast. Your healthcare provider must drain the abscess to treat it and for it to heal.4
Mastitis Symptoms
Mastitis is unique because a doctor commonly diagnoses it by evaluating a mother’s symptoms, which range in severity.1
Symptoms frequently associated with mastitis include the following:2
- Breast pain
- Hot, red, tender location on the breast
- Fever
- Increased heart rate
- Headache
- Muscle aches
- Fatigue (which may last longer than other symptoms)
If you are breastfeeding and have any of these symptoms, reach out to your healthcare team for guidance.
Mastitis Treatment
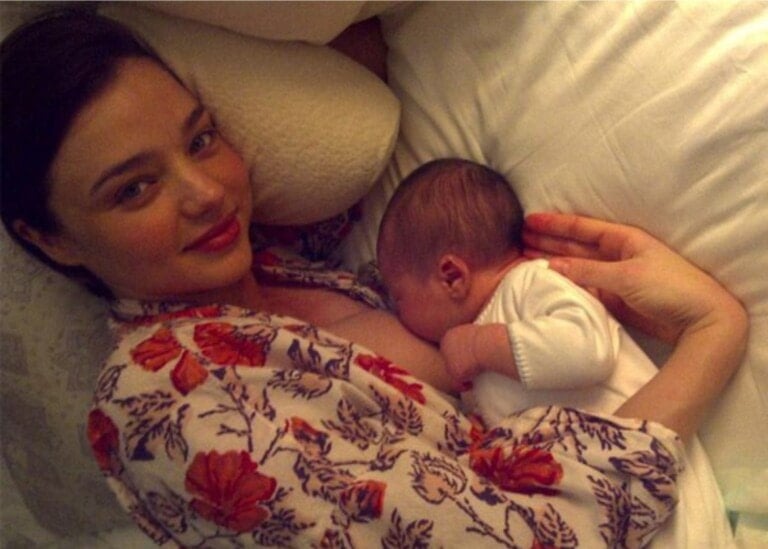
When treating mastitis, you will usually hear similar recommendations across the board. First and foremost is to feed on demand. When your baby shows hunger cues, it’s time to feed. I know what you’re thinking, “I can breastfeed my baby even if I have an infection?” Yes! Breastfeeding with mastitis is safe for full-term, healthy babies and helpful in the treatment process because it means stopping when they are full and avoiding overfeeding.5
When possible, putting your baby to your breast to feed is always recommended versus using a breast pump. It is essential to watch a baby’s hunger cues, feed them when they’re hungry, and stop when they are full. You do not want to overfeed, especially when having mastitis, because overfeeding can cause an increase in milk production, which can lead to more inflammation in the breast. And more inflammation is the last thing you need when trying to get rid of mastitis.4
Over-the-Counter Medications
Mastitis has some very uncomfortable symptoms, and it is crucial to manage them. One helpful intervention is taking over-the-counter medications. These include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen to help with inflammation and acetaminophen to help with pain relief. Taking these as directed can help make you more comfortable, which is key in helping you feel confident and able to continue breastfeeding.4
Ice is also a good idea. Using ice on the breast’s affected area can help decrease inflammation. Previous recommendations were to use heat, but heat can worsen symptoms by causing vasodilation or widening blood vessels, which allows for more blood flow. Not only is ice helpful in decreasing edema and slowing blood flow, but the coolness can also bring comfort.4,6
If symptoms persist and your healthcare provider suspects you have bacterial mastitis, they will recommend antibiotics. Common first-line antibiotics include dicloxacillin or flucloxacillin. Take antibiotics as prescribed and continue the entire course, even if you are feeling better halfway through.4
Additional treatment measures in the ABM protocol include:4
- Sunflower lecithin
- Therapeutic ultrasound
- Probiotics
- Decreasing oversupply of breast milk
If your mastitis becomes a recurrent problem, seek help from your healthcare team so they can evaluate why it keeps occurring.
Could a Lactation Consultant Help Me?
Breastfeeding presents plenty of new challenges, especially when you have mastitis. These problems can include difficulty latching due to engorgement, a baby’s refusal to eat because of a salty taste due to mastitis, and a decrease in milk supply. Working with a lactation consultant can be helpful when navigating these challenges. You can create a plan to help overcome them and meet your breastfeeding goals.5
It is important to note that it is common to see a decrease in milk supply when a woman has mastitis. But this is usually not permanent, and supply can return.4
Preventing Mastitis
While breastfeeding, there are some essential tips and recommendations that can help you to prevent mastitis.3,4
- Downregulate your breast milk supply if you have an oversupply. Because an oversupply of breastmilk leads to inflammation, it can progress to mastitis. It is always a good idea to consult a lactation consultant to devise a plan to decrease your supply safely.
- Wear a supportive bra without an underwire. Underwire can increase pressure on the breasts. This can cause plugged ducts and mastitis. Wearing a supportive bra will help prevent lymphedema and back pain.
- Avoid breast massage. Causing trauma by deeply massaging the breast can cause injury and inflammation in the breast.
Mastitis, Mental Health, and Breastfeeding Goals
Whether you are a first-time mom or a seasoned pro, any unexpected occurrence with a newborn in tow will increase your stress, especially when it comes to feeding your baby. Mastitis can be a mentally exhausting diagnosis to navigate because you are in pain but still need to feed your baby. The situation can feel overwhelming. It’s essential to ask for help during this time, whether extra help around the house from your partner or seeking help from your healthcare team for increased feelings of anxiety or depression.
While navigating mastitis is no walk in the park, you can successfully overcome this nuisance and continue breastfeeding. Being diagnosed with it does not have to be the end of your breastfeeding journey. If you are concerned you might be experiencing signs of mastitis, seek help from your healthcare team and get treatment as soon as possible. You can do this, mama!