When I was expecting, the concept of breastfeeding felt vague and distant. I just knew that moms nourished their babies through their breasts, but there was another choice—formula—that many seemed to prefer.
Naturally, I was a little freaked out about everything from childbirth to changing diapers. I’m someone who attacks fear with knowledge, so I hit the books.
I found clusters of general tidbits about breastfeeding among all the sleep training and diaper-changing advice. I learned that:
- “Mother’s milk is liquid gold.”
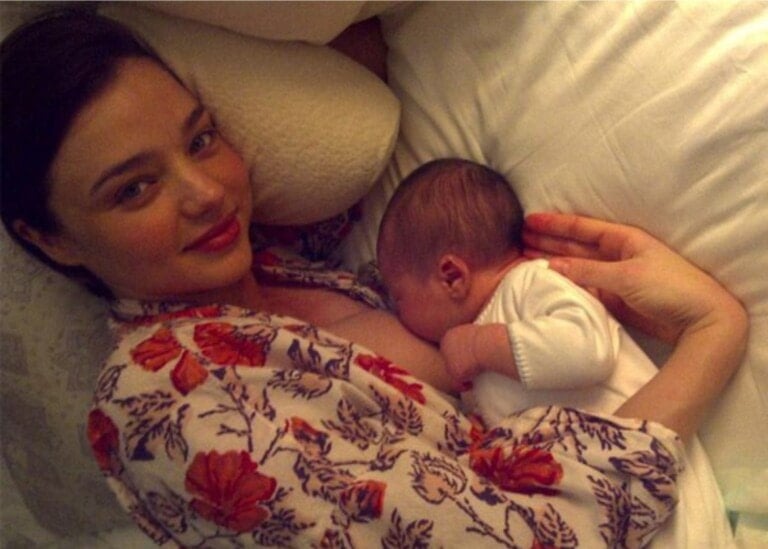
- Feeding promotes a unique bond between mommy and baby.
- Breast milk has all kinds of nutritious advantages over formula.
- It provides babies with these magical, invincible antibodies for protection throughout childhood.
By the end of my pregnancy, I was set on exclusive breastfeeding. It was the path for me. I wanted the very best for my baby. But, frankly, nothing prepared me for how hard and emotionally taxing this journey might be. No one told me it wasn’t smooth sailing at first and that I shouldn’t feel bad if I encountered rough waters. I shouldn’t give up. And I shouldn’t let someone else make a choice for me about how I’d feed my child.
What I Wish First-Time Moms Knew About Breastfeeding
Here’s what I wish first-time mothers knew about breastfeeding. If you’re on the brink of motherhood, I hope this helps you enjoy feeding your baby with more confidence.
Your Milk Doesn’t Come In Right Away
Did you also envision a happy baby who knew how to feed right out of the womb, or was that just me?
Some articles I read painted an image of flowing breastmilk, bonding, and bliss immediately after birth. When this wasn’t the case, I felt like I failed at the whole mom thing right out of the gate.
I thought giving birth would trigger some magical milk switch in my body. I’d set baby to the boob for an endless supply. Instead, I got stitched up after a c-section as my newborn was whisked away to get washed, weighed, and warmed.
My milk didn’t come in that day or the next. It started coming in on the third day, as my doctors pressured me to supplement with formula because “baby needed to eat.”
Sure, baby was getting droplets of liquid here and there, but mature mother’s milk was nowhere in sight. And you know what? That’s okay.
When you first give birth, your breasts let down colostrum, a sticky, thin substance affectionately called “liquid gold.” It’s chock-full of protein and antibodies, and it’s exactly what your baby needs, even if in tiny doses.
If you’re anxious to produce more colostrum, try hand expressing it between feedings. Your nurse or doula can coach you when you’re still in the hospital.
Once you get a few droplets of colostrum through hand expression, feed it to baby with a tiny spoon. Finger feeding is okay as well. Don’t get pressured into supplementing with formula if you plan to breastfeed exclusively. No, your baby isn’t starving, and yes, she’s getting all she needs until your full milk comes in.
Latching Doesn’t Always Come Easy
Newborns have a natural rooting reflex, but they don’t automatically get the latching down. They need some coaching and encouragement.
If you’ve had an unmedicated vaginal birth, direct skin-to-skin with your baby might be possible as soon as he’s born. This promotes latching. Under most circumstances, though, it’s a learning process for both mom and baby.
Since my son was born via c-section, we didn’t have the opportunity for immediate skin-to-skin contact. Like all other newborns whose moms receive pain management meds, he had a little bit of residual medication in his system. Both of those factors probably interfered with latching at first. I didn’t know that having an epidural might affect my baby’s latch.1
Your Medical Support Makes All The Difference
Before we left the hospital, my medical team coached us through the initial feeding phase. But while some of the professionals were eager to help us breastfeed successfully, a few decided that making it work shouldn’t be my priority.
When my son wouldn’t latch on the first day, a nurse gave me a nipple shield to facilitate feeding. I wish I knew that a nipple shield should be used after a few days as a last resort. It can further confuse baby’s latch if introduced too soon. I was scared into supplementing with formula by the third day of my baby’s life. I wish I knew that my milk wouldn’t come in immediately and that bottle feeding would prevent my baby from learning to latch sooner.
A couple of professional angels made it possible for me to feed my son for as long as I did. A seasoned nurse came by on our last night as my fussy baby struggled to latch. She took away the nipple shield and whipped out a small spray pen. She spritzed the shield and gave it back.
“Sugar water,” she said. “You’re welcome.”
That little droplet of sugar water motivated my little guy to wake up and work on his latch.
Consult A Lactation Specialist
My postpartum hospital stay lasted four days. A jaundiced baby and a mama whose blood pressure wouldn’t go down is a recipe for a longer stay. That entire time, I struggled through our latching ordeal. With mixed emotions and disappointment, I tried latching, pumping, and supplementing with formula.
On our last day, my team sent over a lactation consultant . . . What? Is that a thing?
My consultant taught me how to hand express my milk during our visit, which was entirely too short. (It’s more effective than pumping during those first few days.) She showed me how to properly position my baby for breastfeeding, taught me some tricks for waking him up during feedings, and how to tell when he was full.
She talked to me about cluster feedings and was appalled that my doctors made me supplement before they called her in to help. Most importantly, she taught me to speak up for my right to breastfeed. I felt more comfortable with that one professional while feeding my baby than with the various rotating doctors.
When in doubt, ask for a lactation specialist. If your hospital doesn’t have one on staff, ask your pediatrician or doula for recommendations. A specialist is your number one advocate for breastfeeding. She might be just what you need to get to that finish line with confidence.
Dads Can Feed Breastfed Babies
One common reason some moms choose not to breastfeed is that no one else can be in charge of feeding. It’s understandable, honestly. Moms need a break sometimes; a nap here and there while daddy feeds the little one sounds heavenly, for instance.
But guess what? You don’t have to compromise your resolve to breastfeed to let daddy share in the fun. Dads can feed the baby, too, if you can express milk.
Since I was already supplementing with formula, we bottle-fed the milk I pumped. There were better options, though. Bottle feeding a breastfed baby can create nipple confusion. Babies are instinctually resourceful. They don’t want to work for their food if they discover it’s unnecessary. Since milk flows easier from a bottle, babies introduced to that aren’t keen on going back to the breast.
Dads can simulate breastfeeding. According to Metro.co.uk, that’s what a dad did when his wife couldn’t breastfeed due to medical reasons. He got a lot of flack for it on social media, but he wasn’t afraid of the public’s judgment if it meant doing what was best for his baby. This is a genius alternative if your baby’s dad is up for it.
You’re Not A Failure If You Don’t Continue Breastfeeding
In a perfect world, I would have breastfed until my baby weaned, perhaps around a year old. I wouldn’t mind if it were longer than that. But we all know plans and parenting don’t often go hand in hand, right?
My milk started drying up by the sixth month. Between pumping, feeding, and trying to increase my milk supply, I was too exhausted for anything else. My life was all about fenugreek, Mother’s Milk tea, hand-expressing (it’s more effective than pumping sometimes), and marathon breastfeeding sessions with a baby who was increasingly frustrated.
I knew my milk supply was decreasing and that maybe I wouldn’t be able to do much to bring it back up. The truth is, my supply was never so abundant that I could stop supplementing with formula. But as a mom who was desperate to breastfeed, I was in denial.
Then, the feelings of failure flooded over me. How was I unable to feed my child for a full year? Why did I let my supply get so low? How could I give up at this point? It wasn’t fun feeling like a malfunctioning mommy.
I wish I had known then that I was far from a failure. I tried very hard to breastfeed from day one. We both hurtled through some minor medical challenges. I contended with a weak initial support system for breastfeeding. I pumped after each feeding, and when my baby wouldn’t latch, he still benefited from his mother’s milk.
I’m not a failure because I couldn’t continue to breastfeed. Neither are you. If you struggle with milk production, there are options for you to prolong feeding your baby. If you feel like you’ve exhausted every option and you’re just unable to sustain milk production, you aren’t a failure. You’ve given your baby all the milk you can produce, and every bit counts toward her overall well-being. If you still want your baby to benefit from breastmilk, you can look for a local donor’s bank or a mom who produces more than she needs. That’s what I did when I finally accepted that my breastfeeding days were over.
As a new mom, it’s important to arm yourself with information. It’s also great to make goals and picture ideals, but plans don’t always pan out, and breastfeeding is no exception. The best you can do is advocate for your choice to feed your baby and take avenues that enhance your chances of success. That in itself counts as a positive experience.