A common joke in pregnancy is, “Did my water break, or did I just pee myself?” Pregnancy incontinence is real, and it can be funny to joke about! However, knowing if your water has broken is vital to avoid infections like chorioamnionitis. This is especially true if you are not full term or you are full term, but your contractions have not started.
Call your provider or go to the hospital if your water breaks before labor begins. Leaking amniotic fluid puts you at risk of developing an infection called chorioamnionitis. Because it can be severe, it is essential to know what chorioamnionitis is to recognize the symptoms and seek treatment if necessary.
What is Chorioamnionitis?
Chorioamnionitis is an infection of the amniotic sac, amniotic fluid, or placenta. The infection can also spread to the umbilical cord. It happens when bacteria or other germs enter the sterile uterus.1,2,3
What Causes Chorioamnionitis?
Your uterus and baby are typically very protected during pregnancy. The cervical mucus plug and the amniotic sac act as barriers to prevent normal bacteria from crossing from the vagina into the bag of waters in the uterus.2
The placenta also filters to prevent infection from reaching your uterus or baby during pregnancy.4
Chorioamnionitis infection can occur when these barriers, filters, and protections fail. There are three ways of getting a chorioamnionitis infection.
Ascending Chorioamnionitis
Most of the time, chorioamnionitis happens when your membranes rupture, and bacteria find a way to travel up through the cervix and into the amniotic sac. The longer your membranes have been ruptured, the more at risk you are for developing ascending chorioamnionitis.1
Transplacental
In rare cases, chorioamnionitis can be caused because a maternal infection has crossed the placenta into the amniotic sac and to the baby. This is most seen in cases of listeriosis, a food-borne illness caused by the bacteria listeria.1
Medically-Acquired
Diagnostic tests during pregnancy, such as chorionic villus sampling and amniocentesis, present the risk of introducing bacteria into the uterus during the procedure. However, this is uncommon.1
Symptoms of Chorioamnionitis
There are several symptoms of chorioamnionitis.
Maternal Fever
A fever is the body’s response to fighting infection. Any temperature over 100.4 degrees Fahrenheit is considered abnormal during pregnancy, and maternal fever can reflect a case of chorioamnionitis in a pregnant woman. Nearly all cases of clinical chorioamnionitis present with a fever, and many providers require a fever to make the diagnosis.1
Of course, other potential causes of fever must be ruled out, but chorioamnionitis should be suspected and investigated when a pregnant woman has a fever.
Rapid Heartbeat
Infection in the uterus can cause mom and baby to have higher-than-normal heart rates. If the mother has a heart rate above 100 beats per minute or the baby has a heart rate above 160 beats per minute, chorioamnionitis might be suspected.1
Uterine Fundal Tenderness
Because infection in the uterus causes swelling or inflammation, the uterus may be painful or tender to the touch in cases of chorioamnionitis.1
Pain medications, including an epidural, can mask uterine pain. Uterine pain also has other causes, such as placental abruption. Pain and tenderness are more challenging to quantify than fever and heart rate, which makes these symptoms somewhat less helpful in diagnosing chorioamnionitis.1
Foul-Smelling Amniotic Fluid
An infection in the uterus can cause pus to form and can also cause a bad smell. Specific types of bacteria causing chorioamnionitis are more likely than others to cause this symptom. A bad odor is more likely if the infection has been present for a long time. This can sometimes be a problematic symptom for providers to notice.1
How Common is Chorioamnionitis?
Chorioamnionitis is the most common pathology of pregnancy. It affects between 1 to 4 percent of overall births but is much more common in preterm births and births with a premature rupture of membranes.1,5
How is Chorioamnionitis Diagnosed?
Here are ways your medical provider can diagnose chorioamnionitis.
Clinical Signs
Most often, your medical provider can diagnose chorioamnionitis by the presence of telltale signs of the condition. A fever without another known cause is the main sign of chorioamnionitis, but doctors look for the other symptoms listed above. Because symptoms of fever and abdominal tenderness are also common in other conditions, such as appendicitis and urinary tract infections, your provider may need to rule these out before definitively diagnosing you with chorioamnionitis.1,6
Amniotic Fluid Culture
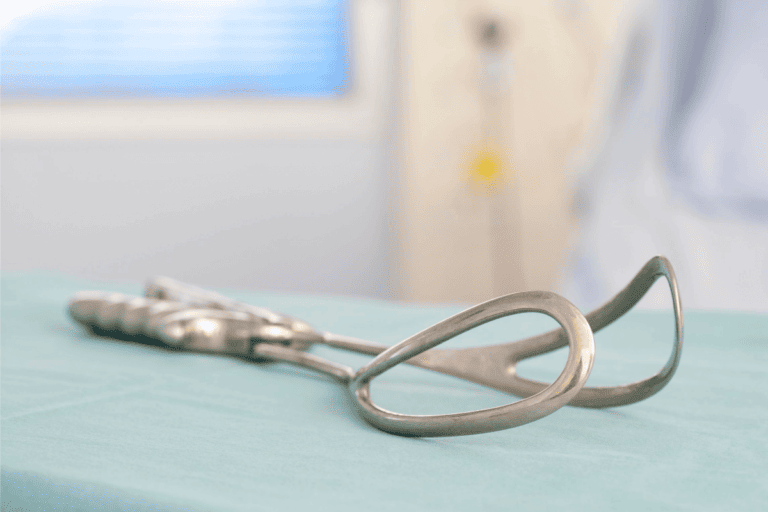
It is possible to diagnose chorioamnionitis by testing amniotic fluid for the presence of bacteria. However, the amniotic fluid must be uncontaminated, so it is usually obtained through an amniocentesis, where a sterile needle is inserted into the uterus to collect amniotic fluid. This is the gold standard for chorioamnionitis diagnosis, but it takes a long time for results and is invasive, so it is rarely done.1
Microscopic Examination
A doctor can look at the cells of the placenta, umbilical cord, or membranes under a microscope for signs of inflammation and infection.5
How is Chorioamnionitis Treated?
There are two main ways to treat this type of infection.
Antibiotics
If you are diagnosed with chorioamnionitis, your doctor will likely recommend around-the-clock IV antibiotics to start immediately and continue until delivery. This treatment decreases the need for prompt delivery, especially if you are still preterm. Antibiotic treatment also reduces the risk of complications for your baby.1
Fever Reducers
In addition to prompt antibiotic initiation, acetaminophen will likely be started to prevent fever since maternal fever can cause swelling of the baby’s brain.1
Can You Prevent It?
There are ways to prevent chorioamnionitis that your medical provider may suggest.
Antibiotics
Just as antibiotics can be used to treat chorioamnionitis, they can also be used to prevent it. If your water has broken and it is not time for you to deliver, your doctor may recommend starting antibiotics to prevent infection from developing.1
Induction of Labor
If your water has broken before labor has begun and you are at least 34 weeks pregnant, labor induction can help prevent chorioamnionitis. This is because the longer your amniotic fluid membranes are ruptured, the greater chance for vaginal bacteria to migrate into the uterus and cause infection.1
What are Possible Complications?
Chorioamnionitis can cause problems for both mother and baby if not diagnosed and managed quickly and properly. Mothers may suffer from postpartum pelvic and wound infections, sepsis, and postpartum hemorrhage.6
Just like their mothers, babies may also suffer from infection and sepsis. If chorioamnionitis causes preterm delivery, they can suffer from eye and lung diseases of prematurity. They can also develop inflammation that can cause cerebral palsy and other neurological deficits.1,6
Chorioamnionitis can be scary and severe if not caught and treated correctly. However, it is very common and often has no long-term effects. If you suspect you are suffering from chorioamnionitis, contact your provider immediately. They will provide a treatment plan to optimize your and your baby’s health and outcomes.